Why Fatigue and Weight Gain Often Mean Mitochondrial Dysfunction
A practical, science-backed look at how broken cellular powerhouses make you tired and heavy — how to spot it, test it, and (safely) start fixing it.
Introduction — tired, gaining weight, and frustrated?
It’s common to blame willpower, hormones, or a slow metabolism when energy dips and pounds creep on. But one root cause that often flies under the radar is mitochondrial dysfunction — when the little cellular power plants make less ATP (the body’s usable energy currency), produce more damaging reactive oxygen species (ROS), and fail to regulate metabolism properly.
In this article you’ll learn what mitochondria do, why their malfunction leads to fatigue and weight gain, how to suspect and test for it, and practical, science-backed steps (including up to five safe products) to help restore cellular energy.
What mitochondria do — the short version
Mitochondria are organelles inside your cells that produce most of the body’s ATP via oxidative phosphorylation. They also regulate reactive oxygen species (ROS), cell signaling, and apoptosis — processes that affect metabolism, inflammation, and tissue repair. When mitochondria work well, you feel energetic and metabolically flexible; when they don’t, your whole system feels sluggish.
Core functions:
- Make ATP to power muscle contraction, brain function, and cellular repair.
- Burn substrates (fat, glucose) in a coordinated way.
- Manage ROS and support healthy signaling for insulin sensitivity and appetite regulation.
Why mitochondrial dysfunction produces both fatigue and weight gain
There are several overlapping mechanisms that explain why broken mitochondria often cause the twin complaints: exhaustion and fat gain.
1. Less ATP = less energy for everything
If mitochondria produce less ATP, muscles tire faster and recovery is slower. This leads to reduced activity and a vicious cycle — less movement → fewer calories burned → weight gain. Fatigue is a hallmark symptom in primary mitochondrial disease and appears in multiple reviews of mitochondrial dysfunction and chronic fatigue. PMC
2. Metabolic inflexibility and impaired fat burning
Mitochondrial dysfunction in adipose tissue and muscle reduces the ability to oxidize fat, shifting cells toward storing fat rather than burning it. Reviews specifically link mitochondrial abnormalities with obesity, insulin resistance and metabolic syndrome. PMC
3. Increased oxidative stress and inflammation
Damaged mitochondria leak electrons that form ROS. Chronic ROS contributes to systemic inflammation, which promotes insulin resistance and central fat deposition. That inflammation also makes you feel tired and sore. (This is a well-described axis in metabolic syndrome research.)PMC
4. Hormonal and signaling disruptions
Mitochondria affect hormones like leptin (satiety), thyroid signaling, and insulin responses. Disrupted mitochondrial function can blunt thyroid and insulin actions, favoring weight gain and low energy. Several reviews tie mitochondrial dysfunction to impaired endocrine regulation. Frontiersin
Bottom line: The same mitochondrial failures that make cells less efficient at producing energy also promote the metabolic changes that favor weight gain — which is why you often see both symptoms together.
Symptoms to watch for — and tests your clinician may order
Not every tired, overweight person has mitochondrial disease. But these red flags make mitochondrial dysfunction more likely:
- Persistent fatigue not relieved by rest, especially with exercise intolerance. PMC
- Unexplained weight gain despite diet changes.
- Muscle cramps, weakness, or delayed recovery.
- Brain fog, poor concentration, and mood swings.
- Multi-system symptoms (digestive issues, neuropathy) that point beyond simple lifestyle causes.
Medical & lab tests
Standard tests can help rule in/out metabolic contributors and hint at mitochondrial issues:
- Basic metabolic panel, fasting glucose/HbA1c — rule out diabetes or insulin resistance.
- Lipid panel, TSH/free T4 — evaluate hormones affecting energy.
- Vitamin D, B12, ferritin — common reversible causes of fatigue.
- Markers of mitochondrial stress (in specialized centers): lactate/pyruvate ratio, muscle biopsy for suspected primary mitochondrial myopathy, genetic testing when indicated. PMC
Work with a clinician experienced in metabolic or mitochondrial medicine if symptoms are severe or multi-systemic. For many people, simple lifestyle and targeted supplement changes can make measurable differences without invasive testing.
Common causes of acquired mitochondrial dysfunction
Aside from rare genetic mitochondrial diseases, many everyday factors can impair mitochondrial function over time:
- Poor diet — chronic overfeeding, high sugar intake, and nutrient deficiencies (e.g., CoQ10, B vitamins, magnesium) impair mitochondrial enzymes.
- Sedentary lifestyle — lack of exercise reduces mitochondrial biogenesis (making new mitochondria).
- Chronic stress & poor sleep — impair repair pathways and deplete NAD+, a vital cofactor for mitochondrial enzymes.PMC
- Medications — statins (can lower CoQ10), some antivirals, and environmental toxins may harm mitochondria. European Journal of Medical Research
- Obesity & overnutrition — promote mitochondrial fragmentation and reduced oxidative capacity in fat and muscle. Recent studies link obesity to mitochondrial fragmentation in adipocytes and reduced fat burning. Nature Metabolism
Evidence-based fixes: nutrition, movement, and targeted supplements
If mitochondrial dysfunction is part of your problem, interventions target three goals:
- Support mitochondria to make ATP (substrates, cofactors).
- Reduce mitochondrial stress (antioxidants, remove toxins).
- Encourage mitochondrial biogenesis (exercise, hormetic stressors, some nutrients).
Nutrition first
Eat for steady fuel and mitochondrial health:
- Prioritize whole foods, modest protein, healthy fats (olive oil, avocados, fatty fish), and low-glycemic carbohydrates.
- Include foods rich in mitochondrial cofactors: oily fish (omega-3s), organ meats/eggs (CoQ10 precursors), leafy greens (magnesium, B vitamins), nuts and seeds (selenium).
- Avoid chronic sugar/carb binges that drive insulin resistance and mitochondrial damage.
Move — especially resistance and interval training
Exercise is the single most powerful stimulant of mitochondrial biogenesis. Resistance training preserves muscle mass (which burns energy), and interval training improves mitochondrial function and insulin sensitivity. Start slow, progress consistently, and pair training with adequate protein and sleep.
Sleep, stress & circadian hygiene
Poor sleep reduces NAD+ and mitochondrial repair. Prioritize 7–9 hours, consistent bedtimes, and manage evening light exposure. Stress management (breathwork, mindfulness) lowers chronic cortisol and inflammation that damage mitochondria.
Targeted supplements with human evidence
Below are supplements with the best evidence for supporting mitochondrial function and reducing fatigue/poor metabolic control. I limit picks to ≤5 Amazon-friendly products (see next section). Each bullet includes a key citation.
Coenzyme Q10 (CoQ10)
Role: electron carrier in the mitochondrial electron transport chain and lipid-soluble antioxidant. Trials show CoQ10 can reduce fatigue and support mitochondrial function in some people. PMC
Nicotinamide riboside (NR) / NMN (NAD+ precursors)
Role: raise NAD+, a core cofactor for sirtuins and mitochondrial enzymes. Human trials show NR/NMN can raise blood NAD+ and improve mitochondrial markers / some functional outcomes. PubMed
Pyrroloquinoline quinone (PQQ) & PQQ+CoQ10
Role: PQQ supports mitochondrial biogenesis in preclinical studies and may complement CoQ10 to both create mitochondria and help them run efficiently. Emerging human data suggests benefit. PMC
Omega-3 fatty acids (EPA + DHA)
Role: reduce inflammation, support membrane integrity (including mitochondrial membranes), and improve metabolic health — useful for weight control and cognitive energy. Clinical reviews show benefits at 1–3 g/day for cardiometabolic endpoints. Sciencedirect
D-ribose (select cases)
Role: five-carbon sugar used in ATP backbone. Some studies suggest D-ribose speeds ATP recovery after repeated high intensity work and can reduce perceived fatigue in heavy training or certain metabolic contexts. Use cautiously (affects glucose measurements). PubMed
Note: Supplements are supportive — diet, sleep, and exercise are the foundation.
Top 5 product picks (kept intentionally to five)
These are popular, well-reviewed, and widely available on Amazon. Always check labels and consult your clinician before starting new supplements.

Doctor's Best High Absorption CoQ10
Ubiquinone/ubiquinol blends with absorption enhancers — commonly used 100–200 mg/day.
View on Amazon
TRU NIAGEN (Nicotinamide Riboside)
Commercial NR product used to raise NAD+; follow label dosing (typical 250–500 mg/day). Consult clinician.
View on Amazon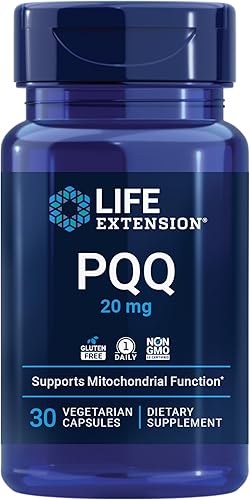
Life Extension PQQ
PQQ to support mitochondrial biogenesis — often used with CoQ10 for complementary effects (10–20 mg/day typical).
View on Amazon
Nordic Naturals Ultimate Omega (or equivalent)
High-purity EPA+DHA fish oil — aim for 1–3 g combined EPA+DHA daily depending on goals.
Search on Amazon
NOW Foods D-Ribose Powder
Used in select cases to speed ATP recovery after intense exercise (start 5 g and monitor).
View on AmazonAffiliate disclosure: Natural Energy Boost may earn a small commission from Amazon links at no additional cost to you. Choose third-party tested products where possible.
Practical protocol — a 12-week starter plan (conservative)
This stepwise approach combines the pillars above. Personalize dose & timing with your clinician.
Weeks 0–2 — foundations
- Sleep: fix schedule; aim 7–9 hours, same wake/sleep times.
- Diet: remove refined sugar, prioritize protein and healthy fats, include oily fish twice weekly.
- Activity: 3× weekly 20–30 min brisk walks + 2 short bodyweight strength sessions.
Weeks 3–6 — add targeted therapies
- Start CoQ10 100 mg/day with a fatty meal.
- Begin omega-3 1 g/day combined EPA+DHA.
- Progress resistance sessions (add weights or heavier reps).
Weeks 7–12 — escalate carefully if needed
- If fatigue persists and under clinician approval, consider adding NR/NMN per label (often 250–500 mg NR) and PQQ 10 mg/day.
- Optional: trial D-ribose (5 g post-workout) if recovery between sessions is slow; monitor blood sugar if diabetic.
Reassess functional changes at 12 weeks: energy, exercise tolerance, waist circumference, resting HR. Consider labs (fasting insulin, HbA1c, lipid profile) to track metabolic improvements.
Real-life examples
Terry Wahls — diet, mitochondria and measurable improvements
Dr. Terry Wahls, a physician who developed the “Wahls Protocol” for mitochondrial support, used targeted nutrition (vegetable-dense, nutrient-rich diets) and lifestyle changes to dramatically improve her own multiple sclerosis symptoms and then studied the approach in clinical trials. Her story is widely cited as an example of how addressing cellular nutrition can improve energy and function. (See Wahls’ clinical work and public writing.) PMC
Celebrity biohacking & NAD+ IVs — why people try it
NAD+ IV infusions and NAD+ precursor supplementation have become popular in celebrity and biohacker circles for perceived energy and recovery benefits. Journalistic pieces describe celebrities and influencers trying NAD+ IV drips for short-term boosts — anecdotal evidence that drives public interest, but clinical certainty is still limited. Use this as inspiration, not proof.PMC
Imagine Sara, a 42-year-old mother who felt exhausted by noon and gained 12 lbs in a year. After baseline labs and a 12-week program (sleep, diet, resistance training + CoQ10 and omega-3), she reported more energy, a 1-inch waist reduction, and could finish a 30-minute walk without needing an afternoon nap. Real change often comes from small consistent steps, not dramatic hacks.
FAQ
How quickly will I feel better?
Some people notice energy improvements in 2–6 weeks (sleep and diet changes often show early benefits). Supplements and mitochondrial biogenesis take longer — 6–12 weeks or more for measurable functional gains.
Are these supplements safe long-term?
Many (CoQ10, omega-3, NR/NMN in trial doses) have reasonable short-term safety data. Long-term effects require more study. If you take statins, blood thinners, or immunomodulators, consult your clinician before starting supplements.
Can I reverse mitochondrial dysfunction completely?
“Reverse” is a strong word. You can often improve mitochondrial function, energy, and metabolic flexibility significantly with nutrition, exercise, sleep, and targeted support — especially when dysfunction is acquired rather than purely genetic.
References &further reading
- Association of mitochondrial dysfunction and fatigue: review summarizing evidence that fatigue is a common symptom in mitochondrial disease and dysfunction. PMC review.
- Mitochondrial Dysfunction in Obesity: review linking mitochondrial dysfunction in adipocytes and metabolic disease. PMC.
- Fatigue and exercise intolerance in mitochondrial diseases: review of symptoms and possible interventions (exercise, CoQ10). PMC.
- Reviews on mitochondrial dysfunction and metabolic syndrome: discussion of oxidative stress, inflammation, and mitochondrial role. PubMed review.
- CoQ10 & mitochondria: 2024 review on CoQ10, mitochondrial dysfunction and clinical evidence. PMC.
- NMN & NAD+ reviews: human trials & mechanistic papers on NAD+ precursors improving mitochondrial metabolism. PMC review.
- Optimized nutrition in mitochondrial disease: trials/clinical guidance linking diet to improved energy and function. PMC.
- Obesity causes mitochondrial fragmentation (2024 Nature article): evidence obesity disrupts mitochondria in adipose tissue.
- NAD+ IV and media coverage: articles covering celebrity interest and current debate on NAD+ therapies. (Journalism pieces summarizing trends.)